Magnetic resonance imaging
"MRI" redirects here. For other uses, see MRI (disambiguation).
| Magnetic resonance imaging | |
|---|---|
| Diagnostics | |
|
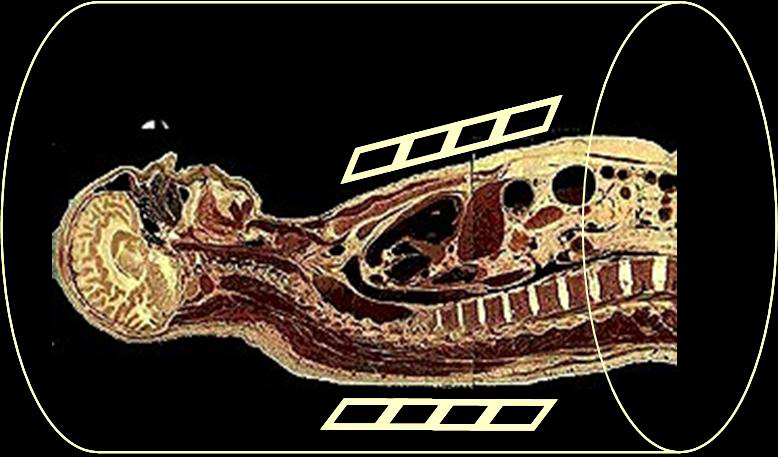
Para-sagittal MRI of the head, with aliasing artifacts (nose and forehead appear at the back of the head)
| |
| Synonyms | nuclear magnetic resonance imaging (NMRI), magnetic resonance tomography (MRT) |
| ICD-9-CM | 88.91 |
| MeSH | D008279 |
| MedlinePlus | 003335 |
Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to image the anatomy and the physiological processes of the body in both health and disease. MRI scanners use strong magnetic fields, radio waves, and field gradients to form images of the body.
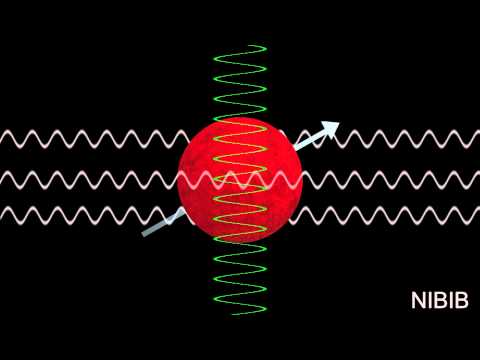
MRI is based upon the science of nuclear magnetic resonance (NMR). Certain atomic nuclei can absorb and emit radio frequencyenergy when placed in an external magnetic field. In clinical and research MRI, hydrogen atoms are most-often used to generate a detectable radio-frequency signal that is received by antennas in close proximity to the anatomy being examined. Hydrogen atoms exist naturally in people and other biological organisms in abundance, particularly in water and fat. For this reason, most MRI scans essentially map the location of water and fat in the body. Pulses of radio waves excite the nuclear spin energy transition, and magnetic field gradients localize the signal in space. By varying the parameters of the pulse sequence, different contrasts can be generated between tissues based on the relaxation properties of the hydrogen atoms therein. Since its early development in the 1970s and 1980s, MRI has proven to be a highly versatile imaging technique. While MRI is most prominently used in diagnostic medicine and biomedical research, it can also be used to form images of non-living objects. MRI scans are capable of producing a variety of chemical and physical data, in addition to detailed spatial images.
MRI is widely used in hospitals and clinics for medical diagnosis, staging of disease and follow-up without exposing the body toionizing radiation.
What is MRI?
MRI is a non-invasive imaging technology that produces three dimensional detailed anatomical images without the use of damaging radiation. It is often used for disease detection, diagnosis, and treatment monitoring. It is based on sophisticated technology that excites and detects the change in the direction of the rotational axis of protons found in the water that makes up living tissues.
How does MRI work?

MRI of a knee
MRIs employ powerful magnets which produce a strong magnetic field that forces protons in the body to align with that field. When a radiofrequency current is then pulsed through the patient, the protons are stimulated, and spin out of equilibrium, straining against the pull of the magnetic field. When the radiofrequency field is turned off, the MRI sensors are able to detect the energy released as the protons realign with the magnetic field. The time it takes for the protons to realign with the magnetic field, as well as the amount of energy released, changes depending on the environment and the chemical nature of the molecules. Physicians are able to tell the difference between various types of tissues based on these magnetic properties.
To obtain an MRI image, a patient is placed inside a large magnet and must remain very still during the imaging process in order not to blur the image. Contrast agents (often containing the element Gadolinium) may be given to a patient intravenously before or during the MRI to increase the speed at which protons realign with the magnetic field. The faster the protons realign, the brighter the image.
What is MRI used for?
MRI scanners are particularly well suited to image the non-bony parts or soft tissues of the body. They differ from computed tomography (CT), in that they do not use the damaging ionizing radiation of x-rays. The brain, spinal cord and nerves, as well as muscles, ligaments, and tendons are seen much more clearly with MRI than with regular x-rays and CT; for this reason MRI is often used to image knee and shoulder injuries.
In the brain, MRI can differentiate between white matter and grey matter and can also be used to diagnose aneurysms and tumors. Because MRI does not use x-rays or other radiation, it is the imaging modality of choice when frequent imaging is required for diagnosis or therapy, especially in the brain. However, MRI is more expensive than x-ray imaging or CT scanning.
One kind of specialized MRI is functional Magnetic Resonance Imaging (fMRI.) This is used to observe brain structures and determine which areas of the brain “activate” (consume more oxygen) during various cognitive tasks. It is used to advance the understanding of brain organization and offers a potential new standard for assessing neurological status and neurosurgical risk.
Are there risks?
Although MRI does not emit the damaging ionizing radiation that is found in x-ray and CT imaging, it does employ a strong magnetic field. The magnetic field extends beyond the machine and exerts very powerful forces on objects of iron, some steels, and other magnetizable objects; it is strong enough to fling a wheelchair across the room. Patients should notify their physicians of any form of medical or implant prior to an MR scan.
When having an MRI scan, the following should be taken into consideration:
•People with implants, particularly those containing iron, — pacemakers, vagus nerve stimulators, implantable cardioverter- defibrillators, loop recorders, insulin pumps, cochlear implants, deep brain stimulators, and capsules from capsule endoscopy should not enter an MRI machine.
•Noise—loud noise commonly referred to as clicking and beeping, as well as sound intensity up to 120 decibels in certain MR scanners, may require special ear protection.
•Nerve Stimulation—a twitching sensation sometimes results from the rapidly switched fields in the MRI.
•Contrast agents—patients with severe renal failure who require dialysis may risk a rare but serious illness called nephrogenic systemic fibrosis that may be linked to the use of certain gadolinium-containing agents, such as gadodiamide and others. Although a causal link has not been established, current guidelines in the United States recommend that dialysis patients should only receive gadolinium agents when essential, and that dialysis should be performed as soon as possible after the scan to remove the agent from the body promptly.
•Pregnancy—while no effects have been demonstrated on the fetus, it is recommended that MRI scans be avoided as a precaution especially in the first trimester of pregnancy when the fetus’ organs are being formed and contrast agents, if used, could enter the fetal bloodstream.

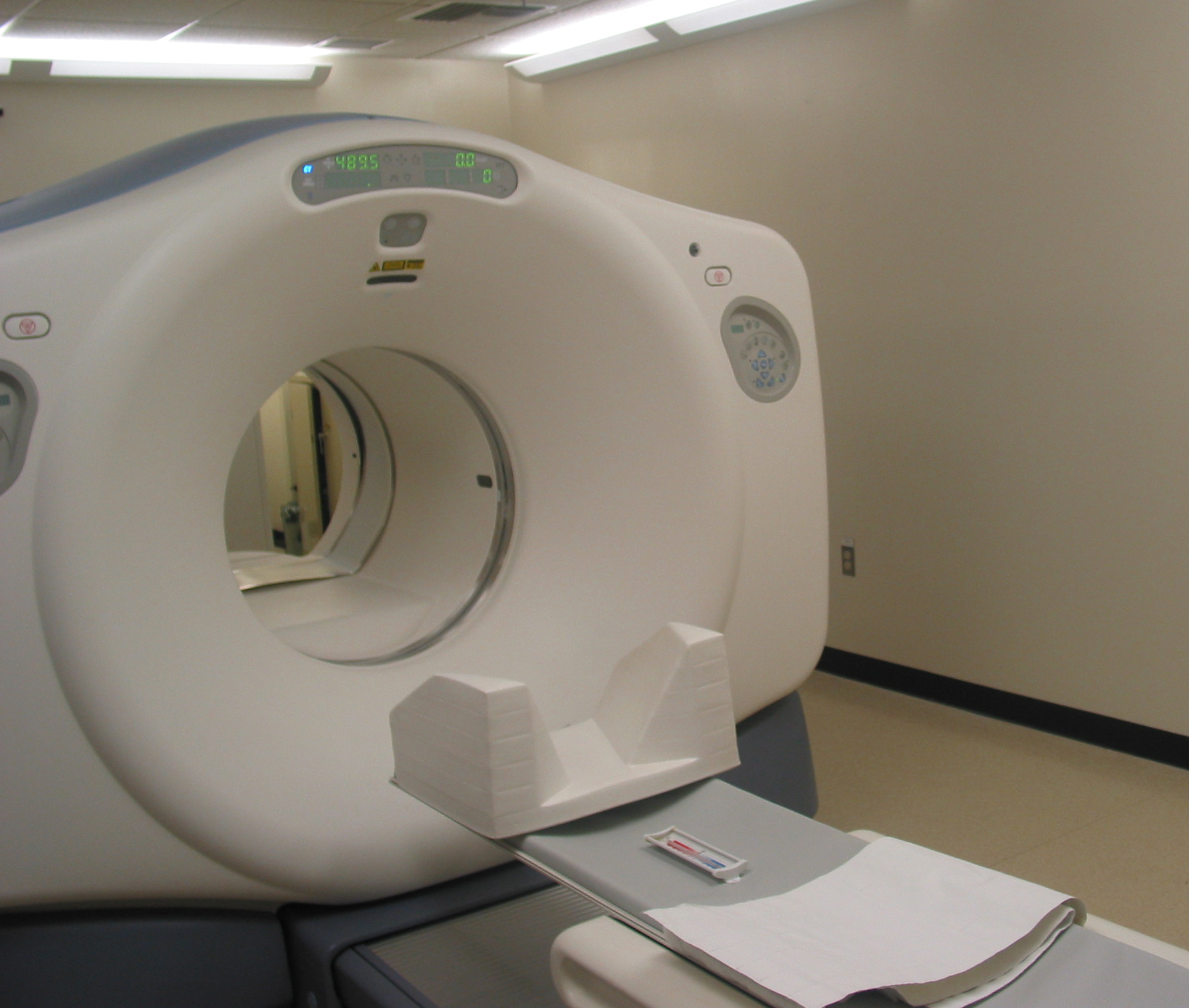
New open MRI machine
What are examples of NIBIB-funded projects in MRI?
Replacing Biopsies with Sound
Chronic liver disease and cirrhosis affect more than 5.5 million people in the United States. NIBIB-funded researchers have developed a method to turn sound waves into images of the liver, which provides a new non-invasive, pain-free approach to find tumors or tissue damaged by liver disease. The Magnetic Resonance Elastography (MRE) device is placed over the liver of the patient before he enters the MRI machine. It then pulses sound waves through the liver, which the MRI is able to detect and use to determine the density and health of the liver tissue. This technique is safer and more comfortable for the patient as well as being less expensive than a traditional biopsy. Since MRE is able to recognize very slight differences in tissue density, there is the potential that it could also be used to detect cancer.
Chronic liver disease and cirrhosis affect more than 5.5 million people in the United States. NIBIB-funded researchers have developed a method to turn sound waves into images of the liver, which provides a new non-invasive, pain-free approach to find tumors or tissue damaged by liver disease. The Magnetic Resonance Elastography (MRE) device is placed over the liver of the patient before he enters the MRI machine. It then pulses sound waves through the liver, which the MRI is able to detect and use to determine the density and health of the liver tissue. This technique is safer and more comfortable for the patient as well as being less expensive than a traditional biopsy. Since MRE is able to recognize very slight differences in tissue density, there is the potential that it could also be used to detect cancer.
New MRI just for Kids
MRI is potentially one of the best imaging modalities for children since unlike CT, it does not have anyionizing radiation that could potentially be harmful. However, one of the most difficult challenges that MRI technicians face is obtaining a clear image, especially when the patient is a child or has some kind of ailment that prevents them from staying still for extended periods of time. As a result, many young children require anesthesia, which increases the health risk for the patient. NIBIB is funding research that is attempting to develop a robust pediatric body MRI. By creating a pediatric coil made specifically for smaller bodies, the image can be rendered more clearly and quickly and will demand less MR operator skill. This will make MRIs cheaper, safer, and more available to children. The faster imaging and motion compensation could also potentially benefit adult patients as well.
MRI is potentially one of the best imaging modalities for children since unlike CT, it does not have anyionizing radiation that could potentially be harmful. However, one of the most difficult challenges that MRI technicians face is obtaining a clear image, especially when the patient is a child or has some kind of ailment that prevents them from staying still for extended periods of time. As a result, many young children require anesthesia, which increases the health risk for the patient. NIBIB is funding research that is attempting to develop a robust pediatric body MRI. By creating a pediatric coil made specifically for smaller bodies, the image can be rendered more clearly and quickly and will demand less MR operator skill. This will make MRIs cheaper, safer, and more available to children. The faster imaging and motion compensation could also potentially benefit adult patients as well.
Another NIBIB-funded researcher is trying to solve this problem from a different angle. He is developing a motion correction system that could greatly improve image quality for MR exams. Researchers are developing an optical tracking system that would be able to match and adapt the MRI pulses to changes in the patient’s pose in real time. This improvement could reduce cost (since less repeat MR exams will have to take place due to poor quality) as well as make MRI a viable option for many patients who are unable to remain still for the exam and reduce the amount of anesthesia used for MR exams.
Determining the aggressiveness of a tumor
Traditional MRI, unlike PET or SPECT, cannot measure metabolic rates. However, researchers funded by NIBIB have discovered a way to inject specialized compounds (hyperpolarized carbon 13) into prostate cancer patients to measure the metabolic rate of a tumor. This information can provide a fast and accurate picture of the tumor’s aggressiveness. Monitoring disease progression can improve risk prediction, which is critical for prostate cancer patients who often adopt a wait and watch approach.
Traditional MRI, unlike PET or SPECT, cannot measure metabolic rates. However, researchers funded by NIBIB have discovered a way to inject specialized compounds (hyperpolarized carbon 13) into prostate cancer patients to measure the metabolic rate of a tumor. This information can provide a fast and accurate picture of the tumor’s aggressiveness. Monitoring disease progression can improve risk prediction, which is critical for prostate cancer patients who often adopt a wait and watch approach.
History[edit]
Magnetic resonance imaging was invented by Paul C. Lauterbur in September 1971; he published the theory behind it in March 1973.[99][100] The factors leading to image contrast (differences in tissue relaxation time values) had been described nearly 20 years earlier by Erik Odeblad (physician and scientist) and Gunnar Lindström.[101][102][103][104]
In 1950, spin echoes were first detected by Erwin Hahn[105] and in 1952, Herman Carr produced a one-dimensional NMR spectrum as reported in his Harvard PhD thesis.[106][107][108] In the Soviet Union, Vladislav Ivanov filed (in 1960) a document with the USSR State Committee for Inventions and Discovery at Leningrad for a Magnetic Resonance Imaging device,[109][110][111] although this was not approved until the 1970s.[112]
By 1959, Jay Singer had studied blood flow by NMR relaxation time measurements of blood in living humans.[113][114] Such measurements were not introduced into common medical practice until the mid-1980s, although a patent for a whole-body NMR machine to measure blood flow in the human body was already filed by Alexander Ganssen in early 1967.[115][114][103][116][117]
In the 1960s and 1970s the results of a very large amount of work on relaxation, diffusion, and chemical exchange of water in cells and tissues of all sorts appeared in the scientific literature.[103] In 1967, Ligon reported the measurement of NMR relaxation of water in the arms of living human subjects.[103] In 1968, Jackson and Langham published the first NMR signals from a living animal.[103][118]
In a March 1971 paper in the journal Science,[119] Raymond Damadian, an Armenian-American physician and professor at the Downstate Medical Center State University of New York (SUNY), reported that tumors and normal tissue can be distinguished in vivo by nuclear magnetic resonance ("NMR"). He suggested that these differences could be used to diagnose cancer, though later research would find that these differences, while real, are too variable for diagnostic purposes. Damadian's initial methods were flawed for practical use,[120]relying on a point-by-point scan of the entire body and using relaxation rates, which turned out not to be an effective indicator of cancerous tissue.[121] While researching the analytical properties of magnetic resonance, Damadian created a hypothetical magnetic resonance cancer-detecting machine in 1972. He filed the first patent for such a machine, U.S. Patent 3,789,832 on March 17, 1972, which was later issued to him on February 5, 1974.[122] Zenuemon Abe and his colleagues applied the patent for targeted NMR scanner,U.S. Patent 3,932,805 on 1973.[123] They published this technique in 1974.[124][114][103]
Damadian claims to have invented the MRI.[125]
The US National Science Foundation notes "The patent included the idea of using NMR to 'scan' the human body to locate cancerous tissue."[126] However, it did not describe a method for generating pictures from such a scan or precisely how such a scan might be done.[127][128] Meanwhile, Paul Lauterbur at Stony Brook University expanded on Carr's technique and developed a way to generate the first MRI images, in 2D and 3D, using gradients. In 1973, Lauterbur published the first nuclear magnetic resonance image[99][129]and the first cross-sectional image of a living mouse in January 1974.[130] In the late 1970s, Peter Mansfield, a physicist and professor at the University of Nottingham, England, developed the echo-planar imaging (EPI) technique that would lead to scans taking seconds rather than hours and produce clearer images than Lauterbur had.[131] Damadian, along with Larry Minkoff and Michael Goldsmith, obtained an image of a tumor in the thorax of a mouse in 1976.[132] They also performed the first MRI body scan of a human being on July 3, 1977,[133][134] studies they published in 1977.[132][135] In 1979, Richard S. Likes filed a patent on k-space U.S. Patent 4,307,343.
During the 1970s a team led by John Mallard built the first full body MRI scanner at the University of Aberdeen.[136] On 28 August 1980 they used this machine to obtain the first clinically useful image of a patient's internal tissues using Magnetic Resonance Imaging (MRI), which identified a primary tumour in the patient's chest, an abnormal liver, and secondary cancer in his bones.[137] This machine was later used at St Bartholomew's Hospital, in London, from 1983 to 1993. Mallard and his team are credited for technological advances that led to the widespread introduction of MRI.[138]
In 1975, the University of California, San Francisco Radiology Department founded the Radiologic Imaging Laboratory (RIL).[139] With the support of Pfizer, Diasonics, and later Toshiba America MRI, the lab developed new imaging technology and installed systems in the US and worldwide.[140] In 1981 RIL researchers, including Leon Kaufman and Lawrence Crooks, published Nuclear Magnetic Resonance Imaging in Medicine. In the 1980s the book was considered the definitive introductory textbook to the subject.[141]
In 1980 Paul Bottomley joined the GE Research Center in Schenectady, NY. His team ordered the highest field-strength magnet then available — a 1.5-T system — and built the first high-field device, overcoming problems of coil design, RF penetration and signal-to-noise ratio to build the first whole-body MRI/MRS scanner.[142] The results translated into the highly successful 1.5-T MRI product-line, with over 20,000 systems in use today[when?]. In 1982, Bottomley performed the first localized MRS in the human heart and brain. After starting a collaboration on heart applications with Robert Weiss at Johns Hopkins, Bottomley returned to the university in 1994 as Russell Morgan Professor and director of the MR Research Division.[143] Although MRI is most commonly performed at 1.5 T, higher fields such as 3 T are gaining more popularity because of their increased sensitivity and resolution. In research laboratories, human studies have been performed at up to 9.4 T[144] and animal studies have been performed at up to 21.1 T.[145]
REFERENCE:
https://www.nibib.nih.gov/science-education/science-topics/magnetic-resonance-imaging-mriPERSONAL OPINION:
In the brain, MRI can differentiate between white matter and grey matter and can also be used to diagnose aneurysms and tumors.The time it takes for the protons to realign with the magnetic field, as well as the amount of energy released, changes depending on the environment and the chemical nature of the molecules.


No comments:
Post a Comment